Introduction
Careful monitoring and adjustment of nutrient intake is among one of the most effective treatments for a variety of metabolic disorders, including obesity. Unfortunately, a majority of individuals enter a state of self-destruction by creating a non-sustainable and nutrient-deficient plan. These destructive actions are then further encouraged by many online influencers, promoting drastic non-scientific methods. These self-destructive patterns and increased food availability have ultimately led to a rise in obesity prevalence throughout most of the developed world, which has resulted in the obesity being the most prominent chronic disease. Besides lifestyle changes, bariatric surgery, the most preferred for patients, has been drastically improved over the years, yet still carries significant risks that can be mitigated through other measures. These measures include personalized nutrition and the use of pharmaceutical aids, with GLP-1 agonists and dual GLP-1/GIP agonists having tremendous therapeutic potential.
This journal review aims at presenting a study that deploys tirzepatide, a dual agonist of the glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptors. Before we discuss the therapeutic efficacy, a brief review of the GLP-1, GIP, and glucose regulation is warranted.
Glucose & Insulin
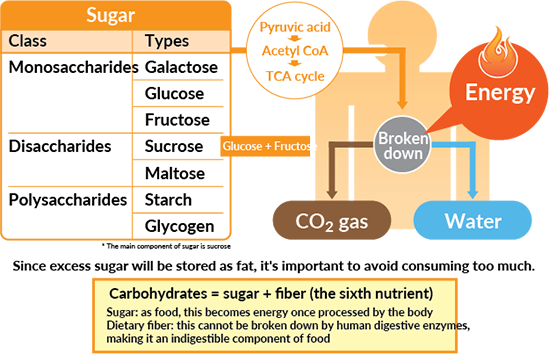
Glucose is the body’s primary fuel source, acting as a necessary molecule for glycolysis which fuels the Kreb’s cycle, and downstream cellular respiration. The intake of simple sugars can be quickly absorbed into the bloodstream, however, complex carbohydrates such as starch, which can be composed of multiple glucose molecules bound together. These complex carbohydrates must be broken down by amylases, released by the pancreas into the small intestine. Once the complex carbohydrates are broken down into the base molecule, glucose, it can be taken into the bloodstream and used by cells for energy. There are many complex systems involved in regulating blood glucose levels, including the release and mechanism of insulin.
As glucose molecules circulate, they enter through a glucose transporter on pancreatic beta cells, which results in the release of insulin. The role of insulin is to bind to the insulin receptor on target cells, which activates a plethora of signaling cascades, one of which is to insert glucose transporters into the cell membrane (GLUT). The GLUT allows the glucose from the bloodstream to enter cells and be used for energy, and without the GLUT protein, glucose cannot be used for fuel. Therefore, insulin is crucial for glucose regulation and cellular energy metabolism, thus its dysregulation is apparent in diseases like diabetes.
Takeaways: Carbohydrates from foods are broken down into their primary components, glucose. Glucose is a major source of fuel for the production of energy, and the consumption of glucose stimulates the release of insulin. Insulin’s role in the body is to decrease blood glucose by allowing cellular uptake of glucose.
Glucagon
When glucose is abundant, insulin stimulates cells to store glucose as glycogen in the liver and skeletal muscle. This stored glucose is incredibly useful for quick energy when glucose consumption is not abundant, such as periods of caloric-deprivation or exercise. During these periods, insulin release is inhibited by the actions of glucagon, released from pancreatic alpha cells. Glucagon’s main role as a hormone is to increase blood glucose when levels are too low, such as during fasting or exercise. To achieve glucose homeostasis, glucagon stimulates the liver to breakdown glycogen, thus releasing glucose into the bloodstream.
Takeaway: When blood glucose levels are low, glucagon is released which acts to inhibit insulin release and increase the breakdown of liver glycogen. The primary role of glucagon is to increase blood glucose levels.
Hormones & Digestion
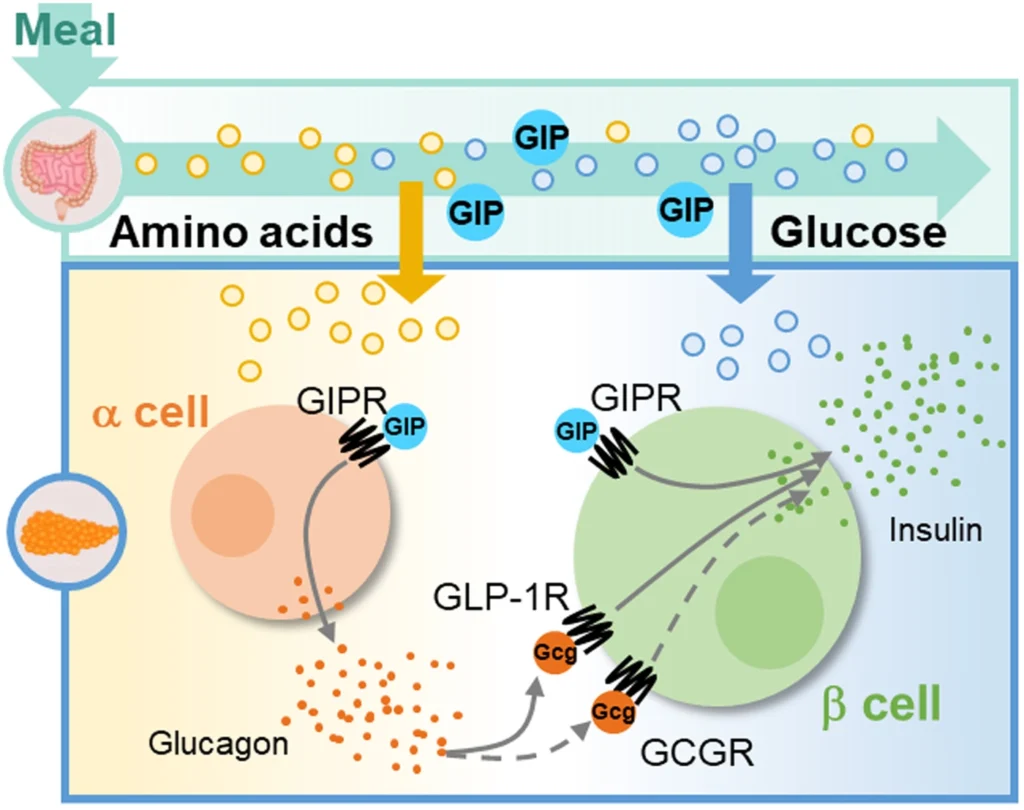
The digestive system is extremely complex, involving a variety of signals originating from the nervous and endocrine systems. Several hormones play a crucial role in regulating glucose, including, as previously mentioned, insulin and glucagon. However, other hormones offer a unique set of characteristics regarding glucose homeostasis, including glucagon-like peptide 1 (GLP-1) and glucose-dependant insulinotropic polypeptide (GIP).
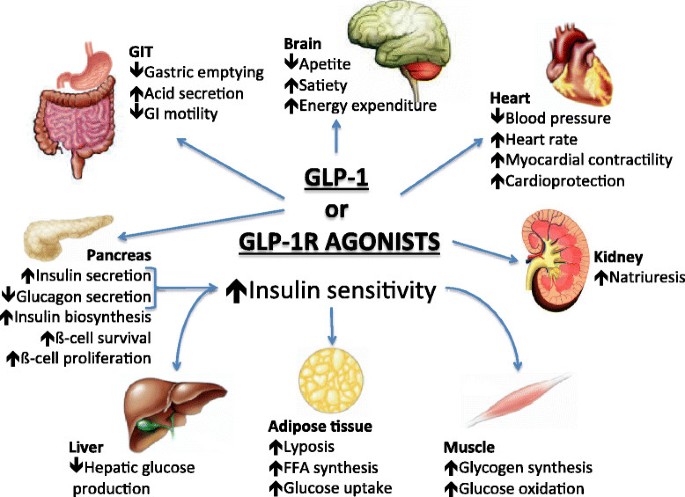
Endogenous GLP-1 is released from cells of the intestine when glucose is sensed and acts primarily to increase insulin secretion, increase insulin sensitivity, and delay gastric emptying. Exogenous GLP-1 receptor agonists exhibit the same effects as endogenous GLP-1, however, modifications can be made to increase time-of-action, thus lowering safety concerns around administration.
Endogenous GIP results in similar physiological changes compared to GLP-1. This includes an increase in insulin secretion and an increase in glucose usage. This hormone also acts to lower blood glucose by stimulating insulin release. GIP also plays a role in altering energy metabolism in the brain, thus making the combination of GLP-1 and GIP favorable for weight loss and treatment of type II diabetes. Exogenous GIP exhibits similar effects as endogenous GIP.
Takeaways: The digestive system is a complex system with a plethora of hormones that regulate satiety, glucose, and gastric motility. Among them, GLP-1 and GIP are important for satiety and glucose homeostasis through insulin release, satiety, and altering cell metabolism.
Obesity
As the prevalence of obesity continues to rise, the number of realized factors involved with the onset also increases. Obesity is characterized by having a body-mass index of above 30 mg/km, or a significantly high percentage of body fat accumulation. At a fundamental level, this is caused by an energy imbalance in which energy intake is greater than energy expenditure. As research continues to improve, genetics, psychology, environment, and hormone imbalances seem to play a large role in the development of obesity. This disease results in dysregulated eating patterns, increased adipose (fat) tissue, increased blood glucose, and increased insulin resistance. Each of these problems has a subset of issues, including an increase in pro-inflammatory fat-secreted hormones and thickened blood from increased glucose levels. To date, the treatment of obesity has been through behavioral clinics and pharmaceutical stimulants, which cause side effects that limit sustained use. Surgical intervention has also been used, with many patients reporting undesired side effects along with a significant price tag. Therefore, a pharmaceutical aide aimed at regulating several pathways, including behavioral and glucose homeostasis, is a favorable therapeutic option in treating obesity.
Takeaways: Obesity is a complex disease involving multi-faceted dysregulation. Hallmark features of obesity include a significant accumulation of adipose tissue along with increase blood glucose levels due to increased insulin resistance. Treatments centered on altering behavior and glucose levels are a promising therapeutic agent.
Tirzepatide Phase 3 Results
Methods
This clinical trial assessed the impact of tirzepatide, a dual GLP-1 and GIP receptor agonist, in obese patients with no history of diabetes. All participants had a body-mass index >30, no history of diabetes, no surgical intervention, and must have reported a previous unsuccessful dietary intervention prior to recruitment. These strict criteria allow the authors to present valid data, since diabetes can strongly influence the action of this drug, and surgical intervention may cause exaggerated side effects.
This phase 3 double-blind, randomized, controlled trial consisted of 2539 participants receiving once-weekly, subcutaneous tirzepatide at 5 mg, 10 mg, or 15 mg or placebo for 72 weeks. To assess the change in various markers, baseline measurements were taken at week 0 and compared to measurements taken at week 72.
Results
The results from this trial are promising for the future of treating obesity. First, all dosage groups receiving tirzepatide experienced a reduction of body-weight with the 15 mg group having the most substantial change in being -20.9%. The 5 mg group displayed -15.0 and the 10 mg group a -19.5 percent change in body weight. There seems to be no significant difference between the 15 mg and 10 mg groups, signifying a plateau in dose-response at around 10 mg.
Along with a significant change in percent body weight from baseline, the following graphs give insight into future dosing regimens. In figure B, the percent change in body weight by week contains a significant drop in weight by all tirzepatide groups from weeks 0 to 12. However, the 10 mg and 15 mg tirzepatide groups displayed a longer period of substantial weight loss, being from weeks 0 to 48 and afterwards plateauing.
- Critical Analysis: A potential use for this therapeutic may deploy 10-15 mg for 48-60 weeks, followed by a rest period of 12-24 weeks for resensitization.
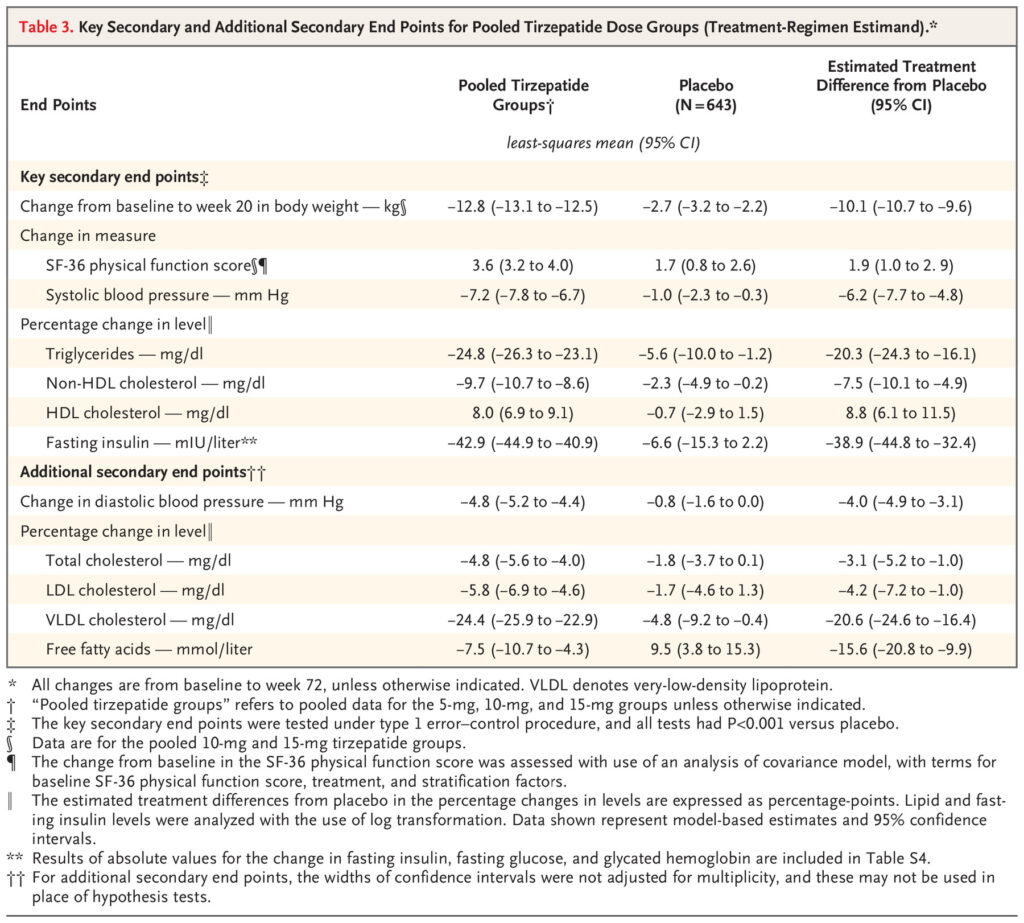
Other data points such as waist circumference, blood pressure, and fasting insulin were favorable after treatment with tirzepatide. Regarding diabetes treatment potential, the tirzepatide group exhibited significantly lower fasting insulin levels, dropping nearly 43% from baseline, with the placebo group only exhibiting a 6.6% decrease from baseline. Other data points that should have been considered for glucose regulation are fasting glucose levels and HbA1c at week 72.
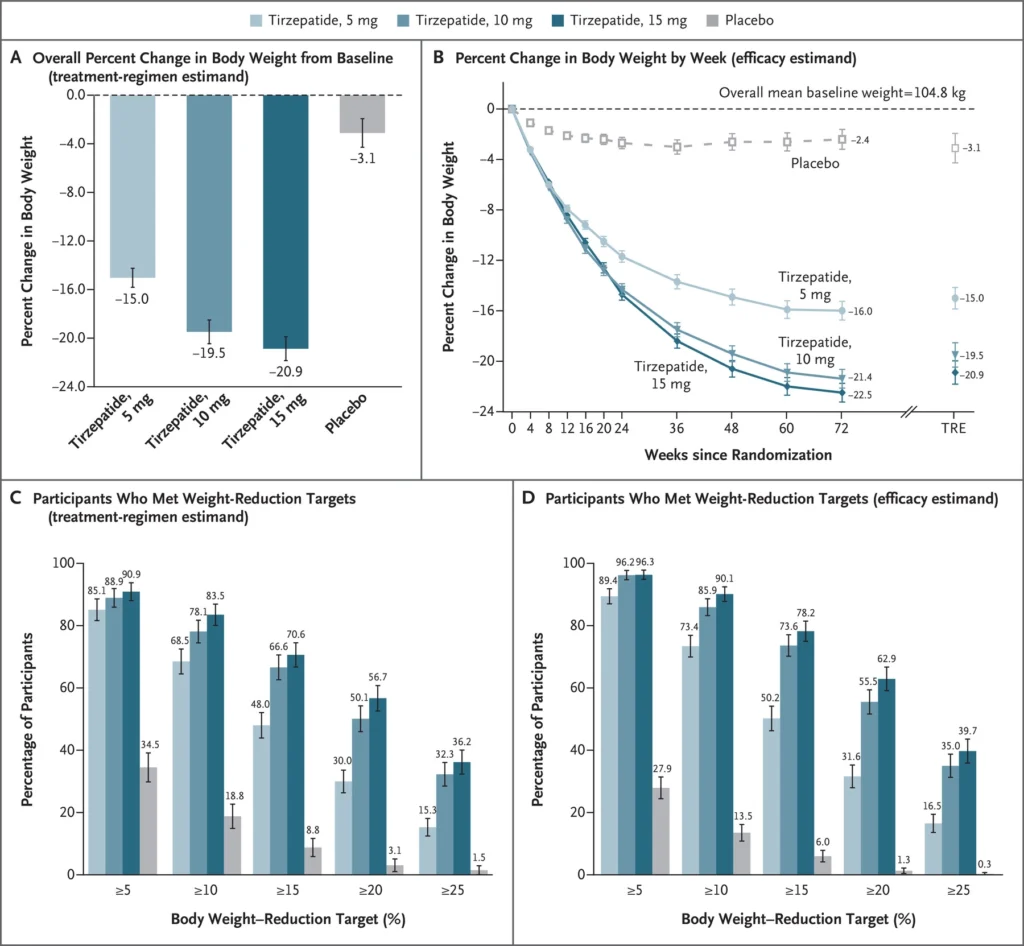
Positive changes in low-density lipoprotein (LDL), high-density lipoprotein (HDL), free fatty acids, and systolic blood pressure were observed in the tirzepatide groups. These measurements, when pooled with the significant decrease in percent change in body weight, indicate that tirzepatide at 10-15 mg is an effective treatment for obesity, although a large population study must be performed to confirm its safety.
Takeaways: Tirzepatide at 10 or 15 mg once-weekly for 72 weeks resulted in a -19.5 or -20.9 percent change in body weight. The usage of tirzepatide also resulted in positive changes regarding LDL, HDL, and systolic blood pressure. The tirzepatide-groups had significantly more reported transient-to-mild adverse effects signifying the dosing protocol had an adequate safety profile.

Discussion
Obesity is the most prominent chronic disease in the world, resulting in an increased risk of cardiovascular disease and diabetes. Unfortunately, treatments have been centered on changing lifestyle habits, which is not a sustainable or realistic ideology for treating a multi-faceted disease involving many feedback loops. Tirzepatide, a peptide with dual agonist activity at the GLP-1 and GIP receptors, exhibits tremendous therapeutic potential. Over the course of 72 weeks, patients receiving a once-weekly subcutaneous injection of tirzepatide at 15 mg exhibited a 20.9 percent decrease in body weight change and positive changes in fasting insulin and lipid profile. The reported adverse effects were primarily transient-to-mild, thus supporting its use as a therapeutic peptide for the treatment of obesity.

Meet the Author
Hello everyone,
My name is Joshua Giblin. I am a post-bachelor researcher/research technician at USC. My interests range from nutrition to nanomedicine and also practical science to improve everyday life. Through this blog, I aim to communicate practical scientific research and present it to curious individuals so that an educated decision can be made. Thank you for reading the blog and showing your support.
Literature cited
- Jastreboff, A. M., Aronne, L. J., Ahmad, N. N., Wharton, S., Connery, L., Alves, B., Kiyosue, A., Zhang, S., Liu, B., Bunck, M. C., & Stefanski, A. (2022). Tirzepatide Once Weekly for the Treatment of Obesity. New England Journal of Medicine, 387(3), 205–216. https://doi.org/10.1056/NEJMoa2206038
Very informative and well-written. Looking forward to reading more from you.